|
The Controlled Substances Act (CSA) has consistently contradicted itself by accepting synthetic THC as medicine (Schedule III) while claiming that Cannabis with THC content greater than 0.3% has no medicinal value (Schedule I). The Department of Health and Human Services (HHS). after a request by the Biden administration, recently pointed out the contradiction to the Drug Enforcement Agency (DEA), the federal agency that enforces the CSA. The DEA is promising a response. As the medicinal acceptance of Cannabis continues to be debated among federal organizations, Medical Cannabis users already have an answer. Cannabis helps cope with cancer. The experience of disease is difficult. Questions of addiction, intoxication, or other socially unacceptable approaches are trivial next to life-or-death questions like, “Will I be alive for the next holiday season?
Despite advancements in pharmacologic and other interventional therapies, a considerable number of cancer patients still suffer from refractory pain. A study, performed in Tel Aviv, Israel surveyed 252 patients with cancer-related refractory pain. The average age of the patients was 62. One hundred and twenty-six of the respondents were using Medical Cannabis and 105 patients were not. That 50% of chronic refractory pain participants report using Cannabis, is a strong indication that Cannabis has medicinal benefits. The study was published in the British Medical Journal Supportive and Palliative Care. Refractory pain is not the only issue. Chronic pain is often accompanied by poor sleep and appetite. Cancer chemotherapy contributes to additional nausea and vomiting. Studies have indicated that Cannabis works as well or better than sleep aids. Scientists even have molecular explanations for the effect of Cannabis on appetite. Additionally, among the chronic pain Cannabis users in this study, almost 70% reported subjective improvements with Medical Cannabis. As well, almost 40% reported significant improvement in coping with the illness. Cannabis is not for everyone. Of the non-users, 65% tried Medical Cannabis and stopped due to a lack of effectiveness (39.7%) or side effects (34.6%). Although, side effects after using Cannabis are generally mild. In this study, no participants required dedicated medical care for side effects after using Medical Cannabis. As the most common side effects, 21.8% reported fatigue and 23.5% reported dizziness . Patients with intractable cancer pain are minimally responsive to many conventional treatments including powerful opioids, adjuvants, and radiotherapy. The authors of this study conclude that Medical Cannabis “… should be considered in addition to current therapies for cancer-related pain and could be offered to patients even earlier in the course of their illness and treatment than is acceptable now.” It’s that time of the year, falling leaves, cool nights, comfort meals, and sleep.
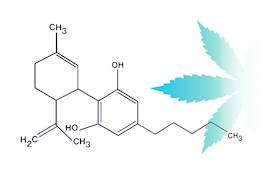
When daylight shifts, so do sleep schedules. We get to bed earlier and sleep later… or so it seems. What’s likely happening is an effect of the clock turned back combined with diminishing sunlight hours. For those who struggle with sleep, it may be a difficult time of year. A recent study published in Exploration of Medicine by the Department of Psychology at Washington State University (WSU), analyzed survey responses from 1,216 people who struggle with insomnia and chose Cannabis to improve their sleep. The surveyed respondents reported that Cannabis helps to relax their mind (83.0%) and body (81.0%). Furthermore, 56.2% reported it helps them get a deeper sleep, 41.6% reported it helps them get a longer sleep, and 36.3% reported it provides them with uninterrupted sleep. Insufficient sleep is recognized as a public health epidemic by the Center of Disease Control and Prevention (CDC). Forty percent of U.S. adults report symptoms of insomnia getting less than the recommended 7 hours of sleep in a 24- hour period. People resort to over the counter (OTC) sleep aids or prescription medicines, which may have a high potential for addiction or undesirable side effects. Participants in the study reported feeling more refreshed, focused, better able to function, fewer headaches, and less nausea the morning after using Cannabis. However, they also reported side-effects common to Cannabis use, excessive drowsiness, red-eyes, dry mouth, and anxiety. Altogether, most respondents chose to use Cannabis every night (68%) and have been using it for more than one year (70%) As with all therapeutic substances, dosage matters. Knowing which Cannabis product to use for sleep requires some understanding of its active product ingredients (API). Cannabis flowers contain, cannabinoids, terpenes, flavonoids, and other potential API. The Cannabis flower contains approximately 20% cannabinoid by weight, mostly consisting of cannabinoids, THC and CBD. Cannabis flowers can be classified into Type I (high THC, low CBD), Type II (equivalent THC and CBD), and Type III (high CBD, low THC). Generally, THC content is considered important for any product made for sleep. However, THC alone might be stimulating. Typically, Cannabis sleep aides will contain an equal amount of THC and CBD. Some might also contain another cannabinoid, CBN, the oxidative form of THC. Terpenes might also contribute to sleep. Many terpene afficionados bring up linalool, a Cannabis terpene also found in lavender and known to have sedative effects. However, most other Cannabis terpenes may be cognitively stimulating. As well, the synergistic effect of combined cannabinoids and terpenes may be energizing. Preliminary results from CESC’s Dosing Project Initiative suggest that Cannabis flowers with attenuated terpenes may be most relaxing and best for sleep. Although most of the WSU study participants smoked (46.1%) or vaporized (42.6%) Cannabis flower, it’s well known that ingesting Cannabis products also works as a sleep aid. Some consumers prefer ingesting as it results in a longer effect and may be useful for those who tend to wake up in the middle of the night. It is not yet clear whether terpenes significantly contribute to the effect of ingested Cannabis and even less clear whether other Cannabis biochemicals contribute. Cannabis products labeled “Indica” or “Sativa” are generally marketed, but unreliable and the designations are unlikely to predict sleep inducing effects. The WSU study contributes to a better understanding of Cannabis consumers and how they use Cannabis to fall asleep. Outdoor Cannabis is harvested in fall and winter, which are great seasons for sleep. Thanks to regulated and improved access, Cannabis products are available in most states as a safer and more effective option for sleep. Choose wisely, know your dose, and happy dreams from MediCann. Not so long ago, young adults were the primary users of Cannabis. Today, women and adults aged 50+ represent the fastest growing group of Cannabis users. An abstract recently presented at the 2023 Annual Meeting of the Menopause Society in Philadelphia confirmed frequent use of Cannabis by midlife women, particularly to manage an array of menopause symptoms.
Cannabis use is increasing across all age groups. Lack of research puts us in a knowledge gap. Earlier studies largely focused on the Cannabis use habits of men and younger adults. Until now, little was known about the prevalence of Cannabis use among women in and after menopause. Based on data from more than 5,000 midlife women, this new study analyzes the frequency, forms, and motives of Cannabis use in post-menopausal women. Over 40% of the women reported ever using Cannabis most often for chronic pain (28%), anxiety (24%), sleep problems (22%), and stress (22%). Six percent of women reported using Cannabis specifically for menopause, targeting menopause related mood and sleep difficulties. It was noted that ten percent of the study participants used Cannabis in the past thirty days, most often smoking (56%), ingesting edibles (52%), or using Cannabis in more than one form (39%). Thirty one percent reported smoking Cannabis on a daily or near daily basis and 19% reported daily or near daily use of edibles. Dr. Carolyn Gibson, lead author and health services researcher at the University of California, San Francisco explains, “We know that Cannabis products are being marketed to women to manage menopause symptoms and these study findings suggest that midlife women are turning to Cannabis…” This observational study documents that midlife women with menopausal symptoms benefit from Cannabis use. “These findings highlight the need for recognizing and discussing Cannabis in the health care setting,” suggests Dr. Stephanie Faubion, Medical Director of the Menopause Society. After three months, the Australian QUEST Initiative demonstrates that Cannabis improves the quality of life of patients with chronic health conditions.
As Cannabis use increases, questions arise as to the overall benefits of the plant. Public health authorities highlight increasing calls to poison control centers and emergency department visits. The National Institute of Drug Abuse stubbornly holds on to a failed war on “drugs” by questioning the incidence of psychological disorders among young Cannabis users. These claims are reminiscent of Reefer Madness. As with most controversial topics, there is equal or better evidence contradicting the claims. NIDA Director, Dr. Nora Volkow, might retort that studying benefits of Cannabis is not a directive. Whether NIDA's directive is valid (or not), what’s clear is that Cannabis will never go away. It's use improves health and wellness. The U.S. Cannabis community is accustomed to consuming the flower. In the U.S., Cannabis flowers are approximately 60% of sales. Cannabis flowers are difficult to prescribe. Due to variable active constituents, most flower users must apply trial and error to determine an appropriate dose. Flower consumption includes a broader spectrum of terpenes, thiols, esters, and flavonoids, constituents beyond cannabinoids. South of the equator, Australians acknowledge Cannabis use for health and wellness. Although Cannabis flower is available in Australia, researchers at the University of Sydney prefer to study the effect of a more standardized and predictable Cannabis oil. Australian physicians prescribe the oil for chronic conditions involving pain, anxiety, and depression. The oil is extracted from the flower and dispensed by dropper. The products consist of different ratios of THC and CBD in a base of medium chain triglycerides (MCT). For the QUEST initiative, physicians and patients choose four different oil formulations, including 1:20 (1 mg THC and 20 mg CBD per 1 ml), 1:1 (10mg THC and !0 mg CBD per ml), 20:5 (20 mg THC and 5 mg CBD per 1 ml), and CBD 50 (50 mg CBD per 1 ml). The Initiative evaluates patient reported outcomes from 2327 patients prescribed Cannabis oil. The patients completed a baseline and at least one follow-up survey. The average age of the participants was 51 years old, 63% were female and 37% were male. Due to their illness, 25% of the participants were either unemployed, on leave, or on limited work duties. Analysis of the data describes significant and rapid initial improvement of health-related quality of life measures maintained over three months. Pain, fatigue, anxiety, and depression all improved. However, respondents with sleep disturbance or diagnosed with insomnia did not demonstrate statistical improvement. Most of the elderly suffer from chronic pain which significantly alters daily activities and imposes a burden on health care costs. As a poor alternative, opioids lead to serious adverse events including respiratory depression and death. Anxiety and depression symptoms impair work and social functioning. In the past fifty years, despite economic growth, quality of life in the US has declined. Cannabis prohibition accounts for a minute fraction of time. US HHS Secretary Xavier Becerra’s recent recommendation to re-schedule Cannabis under the Controlled Substances Act is an indication that a century of Cannabis prohibition is nearly over. We have evolved with Cannabis. Admittedly, panaceas don’t exist. But, if we have to select a solution or remedy for all difficulties or diseases, Cannabis might be second only to water. Meanwhile, this Australian study from provides real-world evidence to quiet dissenters. Currently, 38 states have Medical Cannabis laws, and 23 states have adult recreational laws. Whether smoking a joint to relax after a hard day of work or ingesting Cannabis oil to stop seizures, it’s clear that many consumers benefit from the health and wellness effects of using Cannabis.
A few decades ago, public attitude regarding Cannabis shifted. The notion that sick people should be allowed to use a relatively safe plant signaled the beginning of the Cannabis movement. Compassion, caregiving, and community were hallmarks. However, issues of access, safety, and consistency arose as the Cannabis industry transitioned from traditionally illegal exchange to tested, regulated, and taxed Cannabis sales. In time, consumers did not want to justify their use to a profession of uninformed and inexperienced healthcare professionals who had ignored Cannabis science despite its apparent usefulness. Consequently, recreational or adult use laws were implemented. How have the recreational laws affected access by Medical Cannabis users? Below are three stories from three different states (two states and D.C.) that highlight how recreational laws may have affected Medical Cannabis users. The first story is from Michigan with a headline that reads “Medical Cannabis Pioneered Legal Weed in Michigan. Now it’s Withering Away.” by Dustin Walsh from Crains Grand Rapids Business. In Michigan, medical Cannabis sales are down 71% from one year ago and 86% from two years ago. The average cost of an ounce is down 52% over the last year to $102. While the medical market declines, Michigan’s adult use market is hitting new heights selling $270 million in July alone and expecting to surpass $3 billion this year, second only to California’s market. Ankur Rungta, CEO of C3 Industries, a vertically integrated operator with 13 high profile dispensaries, explains, “For medical [sales] to really drive a comeback there would need to be differentiation. It’s the same product on both sides (medical or recreational).” Rungta believes that the medical market won’t revive until more research is done on Cannabis products. The second story is from Minnesota, with a headline from MinnPost. “With Legalization of Recreational Cannabis What Does That Mean for Medical Cannabis in Minnesota,” by Peter Callahagn. The story features Minnesota patient Patrick McClellan, who is excited to be installing a hydroponic system to grow his own home Cannabis. “Home grow is a game changer for patients,” says McClellan. With the passage of new recreational laws, Minnesota Medical patients have ended up with the best of both worlds. A recent law will improve access and possibly lower prices for all consumers. “Patients who have been going to two medical providers for the last nine years have been extremely limited,” says McClellan. RISE, owned by Green Thumb Industries (GTI) and GREEN GOODS, owned by Vireo Health, are the only two medical Cannabis operators in Minnesota with 8 stores each throughout the state. The new recreational bill increases access by adding more dispensaries. It was also designed to limit the market dominance of the two main operators, but a lobbying effort by GTI and VIreo convinced legislators to maintain vertical integration and allow the two largest organizations to also sell to the recreational market. “Our medical market is already pretty small,” explained State Representative Zack Stephenson. “We risked losing a medical industry all together.” The third story is from the Washington Post where the headline is “Learning the Highs and Lows of D.C.’s Medical Cannabis Lingo,” by Courtland Milloy. The author is touring a DC dispensary called Anacostia Organics in the Southeast of Washington D.C. In DC, patients pay $30 to get a self-appointed Medical Cannabis card. This past July neighboring Maryland passed a recreational law. According to dispensary owner Linda Mercado Greene, “People from DC began going to Maryland because they could buy Cannabis without spending $30 for a medical card.” (Although, carrying Cannabis across state lines is a federal offense.) Referring to Maryland’s law, Greene says, “It’s kicking our buts, but we hope things will even out soon.” Although products are the same in both recreational and medical Cannabis industries, these laws have had different effects in each state. There doesn’t seem to be much distinction between the two industries except for what laws and regulators make of it. In our exuberance for legalization, have we created a distinction between recreational and medical Cannabis that doesn’t exist? From medical to health and wellness to consumer product good industries, what we all sorely missing is more Cannabis research and education. People know why they use Cannabis. Because of a relatively good safety profile people can use it without judgment, oversight, or adverse effects. Rather than guidance by a medical industry influenced by profit over science, consumers can now grow their own. Meanwhile, it doesn’t hurt to follow the science as we apply new analysis to an old plant. Opioid overdose deaths in the United States continue to rise. Last year, opiate overdoses toppled over 100,000 for the second year in a row. Sixty-eight percent were due to synthetic opiates, mostly fentanyl. We place our trust in the FDA and the pharmaceutical industry to inform us of impending dangers from drugs. Yet, our trust waivers as it’s revealed that pharmaceutical companies, like Purdue, and its owners, the Sackler family, played a “special role” in initiating the current opiate crisis by pursuing a marketing approach that persuaded the medical establishment to widely prescribe opiates. Decades later highly addictive synthetic opiates, like fentanyl, are fueling the crisis and addiction demands the supply of opiates from unregulated markets.
Opiate addicts are pivoting to accessible Cannabis in places where its legal. Researchers at the University of British Columbia and UCLA teamed to investigate the success of this harm reduction strategy. 205 people who use unregulated “street” opioids were selected to complete a Cannabis questionnaire. 118 participants (57.6%) reported using Cannabis to manage opioid cravings resulting in a significant reduction in their opioid use. The researchers concluded that improving the accessibility of Cannabis may be a useful strategy to mitigate the associated harms of the current opioid epidemic. The biochemical explanation for addiction involves dopamine, a neurotransmitter also referred to as the “pleasure chemical.” In response to using pleasurable drugs or after pleasurable experiences, dopamine is released into the neural pathways of the brain’s reward center. The drug or experience is not physiologically damaging. Abuse occurs when repetitive use or behavior cannot be stopped to the detriment of imperatives. The release of dopamine after a pleasurable experience reinforces its behavior by enhancing the memory of the experience noting associated environmental cues. As such, the “pleasure chemical” is a misnomer. Dopamine doesn’t cause pleasure; it reinforces experiences. At appropriate doses, THC and CBD release dopamine into the mesolimbic reward pathways. Endocannabinoids also modulate the neural reward pathway. Cannabinoid and dopamine receptors exist as a heterodimer complex, a unified receptor system. As such, the Endocannabinoid System and its association with dopamine provide an opportunity to moderate addiction. Opiate addicts have already exploited this opportunity by choosing Cannabis to reduce their cravings. There is a general belief in the Cannabis community that smoking Cannabis with a particular “fuel” or “gassy” aroma is most useful in opiate withdrawal. This aroma classification of Cannabis suggests the hypothesis that Cannabis constituents may be acting synergistically. Using an algorithm, the CESC, a Cannabis research organization, classifies Cannabis associated with aroma. The content data derived from a broad analysis of Cannabis is incorporated in the classification and used to determine which Cannabis subtypes effectively modulate behavior. Results of the investigation will benefit current victims of the opioid crisis. The study of community users plays an important role in the development of safe and efficacious Cannabis products. The Cannabis community sits on the front lines of trial and error. Their observations suggest that Cannabis subtypes matter. As a result, multi-agent pharmacology must be applied to derive the optimal qualities of Cannabis keeping in mind that the primary objective is to reduce opioid deaths. A survey administered to military veterans over a nine-month period concluded that their Cannabis use improved their quality of life and reduced their medication use. It’s estimated that twenty percent of 19 million US Veterans have a mental illness or substance use disorder. Included are veterans with depression, anxiety, and PTSD.
This study analyzed survey data from 510 US military participants. The researchers were from the Cannabis Center of Excellence, the University of Utah, and the University of Massachusetts, There are two general approaches to research. The first applies inductive rationale to develop a hypothesis. You might remember 7th grade science when you were given two different chemical substances and asked to write down your observations. Both substances were white, but one was powdery and clumped with moisture the other was crystal-like and dissolved with moisture. You used your inductive rationale or power of observation to determine that the chemicals were different. Observational studies develop theories or hypotheses. The second approach to research applies deductive rationale to test the hypothesis developed from the first approach. You might have hypothesized that the chemical substances tasted different and then put a little in your mouth. One substance tasted like flour and the other tasted like sugar, proving your hypothesis. Cannabis research is much the same. Most scientist are applying inductive rationale or observational study to develop theories. As Cannabis products become more accessible, future studies will test the hypotheses using clinical trials. The Controlled Substances Act (CSA) currently restricts access to Cannabis for clinical trials. In this inductive observational study, 91% of those surveyed reported that Cannabis use improve their quality of life. 80% had fewer psychological symptoms and 73% had fewer physical symptoms. Furthermore, 21% reported using fewer opiates, 30% used fewer over the counter medicines, and 25% had reduced their anti-depressants. Regarding lifestyle, 46% reported consuming less alcohol and 24% less tobacco. Even to a 7th grade scientist, the hypothesis or theory should be clear. It’s been demonstrated on the molecular level how cannabinoids, one of the active ingredients in Cannabis, might reduce pain or improve moods. This study concludes that Cannabis use is associated improved quality of life and fewer mental and physical symptoms. The authors suggest that medical Cannabis use among veterans may have a role in harm reduction. Deductive studies are the next step, where double blind, randomized controlled trials can be used to guide Cannabis dosage, safety, and efficacy. When it comes to proving that Cannabis works as medicine, scientific studies are well on their way. Unfortunately, government regulators are lagging. Delaying rescheduling or de-scheduling of Cannabis ignores the science. What do you think? Is this the evidence that finally convinces government regulators to release the reigns on Cannabis research? Will regulators finally change the status of Cannabis under the CSA? A 7th grader would say yes. Is getting high important for feeling better? A new study titled “Understanding Feeling High and its Role in Medical Cannabis Patient Outcomes” was recently published in the journal “Frontiers in Pharmacology” by researchers at the University of New Mexico. The study found that patients who reported feeling high also experienced 7.7% better symptom relief than those who did not report feeling high. Does getting high contribute to medical treatment? The researchers at UNM are the first to ask the question.
1,882 people recorded the results of 16,480 Cannabis using sessions. That calculates to an average of just more than eight recorded sessions over almost five years. Generally, I see this as a red flag. Most regular Cannabis users use daily to weekly. This study population is clearly different. The respondents reported feeling high 49% of the time. That’s an encouraging result. I would estimate, conservatively, that 75-80% of my patients are getting high. As Cannabis becomes popular and its medical benefits are realized, users may not wish to “get high” thus reflecting this study population. In this study, patient who got high reported 4.4% greater positive effects like “Relaxed” and “Chill”, as well 14.4% increase in negative effects like “Dry Mouth” and “Red Eyes.” “Feeling high is poorly defined in the scientific literature,” explains senior author and associate professor of psychology, Jacob Vigil, “but it is generally associated with both impairment and feelings of euphoria. Typically, feeling high is assumed to be the goal of recreational use, but a limitation to Cannabis therapeutic potential. In this paper we test the validity of this assumption and find that feeling high may be an unavoidable component of using Cannabis medicinally. “ Definitively, this study found a positive association between feeling high and symptom relief. The analysis controlled for THC and CBD levels, dose, mode of administration, and symptom severity. There were other interesting associations. Smoking a pipe appears to be a better predictor of symptom relief than either smoking a joint or vaporizing the flower. However, the major discovery of this study is that higher THC levels are not significant predictors of symptom relief and only become significant once feeling high is included in the analysis. As well, THC is a significant and independent predictor of negative effects. These results suggest that feeling high may be a fundamental component to effectively using Cannabis as medicine. It's all in your head, some might say. They may partially be right. The benefit of Cannabis includes a neuro-emotional component. Thus, a better perspective may be not to separate emotions from physiology. The nexus of the two worlds appears to be where Cannabis has its influences. Our Cannabis research group, the CESC, describes the challenges of understanding Cannabis therapeutics as the “many-to-many problem.” The study’s lead author and associate professor of economics, Sara Stith, also highlights the challenges of using Cannabis as medicine. “Cannabis products are extremely variable in their phytochemical composition and patients vary extensively. These complexities suggest that the future of Cannabis-as-medicine lies in highly customized treatments rather than the conventional pharmaceutical model of standardized dosing.” This study concludes with some important recommendations.
But Are the Costs Sustainable? What happens early, happens often. In California, we’ve realized for quite some time that Cannabis is effective medicine. Our laws have progressed to make Cannabis more accessible, yet some things haven’t changed. Cannabis patients continue to exchange personally grown Cannabis at a high rate. Personal gardens are an immediate solution to high cost, low quality dispensary products. Can’t start a garden or don’t have a green thumb? Find a neighbor who is willing to share or better yet, sign up for a MediCann Membership and join their Patient Exchange Program.
Researchers in New Zealand are just discovering what we already know in California. They interviewed 213 people enrolled in New Zealand’s Medical Cannabis program. Participants were asked about the quality of Cannabis they used and its effectiveness. Findings were published in the journal Drugs, Habits, and Social Policy. As high as 96% reported that cannabis helped them with their medical conditions. Almost half (49%) said they were able to reduce or stop taking prescription drugs. Sounds to me like competition for the pharmaceutical industry. The most common therapeutic use of medical cannabis was pain relief where 96% of participants said it helped reduce their pain. Cannabis also helped those who had difficulty sleeping (97%) and those with mental health issues (98%). Of the participants who took Cannabis for other reasons, such as autism, attention deficit disorder, post-traumatic stress disorder, and difficulty eating, 98% found it helpful. According to co-author Geoff Noller,"This both reinforces that they experienced some actual effect from using Cannabis in that they ceased or decreased other medications with recognized efficacy, and in the case of many of these other medications, they reduced their use of potentially more problematic medications.” Do we need more study? Sure. But the empirical evidence is clear. As medicine, Cannabis works. Many New Zealanders find medical cannabis difficult to obtain, relying on the personal or illegal market. According to another study, only 6% of Kiwis who use Cannabis acquire it through their medical cannabis program. Many New Zealand doctors won’t prescribe medical cannabis. There are a limited number of products on the market, keeping prices high. CBD oil in New Zealand can cost a patient $150-350 per month, with other Cannabis products costing even more. "At present, current regulations create problems for many New Zealanders who otherwise report positive benefits from their use of medicinal cannabis,” says Noller. In my opinion, Cannabis users are spun by mainstream industry that has yet to decide how to capitalize. Legal products are scarce, in poor quality, and their costs are high, in New Zealand, in California, everywhere. The current cost of one gram of flower per day can be on average $300 per month or more. According to CESC Dosing ProjectTM results, pain or disordered sleep best improve with a smoked or vaporized dosage of 1 gm. These costs are not sustainable for those with low means and who require treatment every day. Some of us may recall the “Just Say No” campaign. It started in 1984, an illustrious year highlighted by George Orwell’s literary depiction of government-industrial control. Emerging across the bay from where I’m just now sitting at Oakland, California’s Longfellow Elementary School, the “Just Say No” campaign was instituted by former actress and first lady Nancy Reagan. Speaking with school children, she introduced the “Just Say No” phrase to deter people from using street drugs, including Cannabis. She subsequently travelled to drug rehab centers, wrote guest articles, and appeared on numerous talk shows promoting the “Just Say No” message. Her relentless marketing caught on and spread internationally.
The “drugs” referenced in the “Just Say No” campaign were illicit drugs. In that era, prescription drugs were not targeted with respect to the medical industry. Fast forward 40 years… The children who heard the former first-lady’s speaking are now middle-aged adults. Prescription drugs are known to cause significant damage. After heart disease and cancer, adverse prescription drug effects are the third leading cause of death in the US and Europe. The Fentanyl overdose epidemic accounts for one in five deaths among young people in California. On the other hand, Cannabis advocates celebrate a 4.5-fold increase in Medical Cannabis from 2016 to 2020. The decade appears associated with a trend toward experimenting with plant-based alternative to health and wellness. Most research on the benefits of Medical Cannabis focuses on specific symptoms, like pain and sleep, or how Cannabis lowers the use of opioid prescriptions. A recent Australian study published in the Journal of the American Medical Association Open Network pivoted, focusing on generalized Quality of Life (QOL) measures among patients enrolled in Medical Cannabis Specialty Clinics. 3,148 patients with an average age of 56 participated in this study; that means they were all children during the “Just Say No” years. Most of the patients had chosen Medical Cannabis due to chronic pain, anxiety, or sleep. The principle investigators evaluated QOL measure every three months up to 15 times over a four-year period. Due to a paucity of clinical trials, it’s difficult to claim that a specific Cannabis formulation or active ingredient treats a specific medical condition. Despite hundreds of active ingredients, THC and CBD are the only FDA approved constituents derived from the Cannabis plant. Meanwhile, there are many multi-agent products being used for a wide variety of symptoms or conditions. It’s what our research group terms, the “many to many problem”. Our solution casts a wide net, initiating broad generalized studies to determine what patients use and how the Cannabis products affect Quality of Life. This study does just that. The study used a 36-item short form health survey with 8 distinct scales including questions on physical activity, mental health, social activities, vitality, pain, and general perception of health. Most of the participants were ingesting capsules with varied concentrations of THC and CBD. Very few also reported smoking the Cannabis flower. Starting at low doses and increasing to optimum effect, the average CBD dose climbed to 72 mg per day and stayed relatively the same throughout the four years. The mean THC dose increased throughout the four years from 6.5 to 25.8 mg per day. By the end of the study, only two serious adverse events were noted. QOL scores range from 0-100, where a 10-point change is considered clinically significant. These results demonstrated improvement in QOL with scales ranging from 6.6 to 18.31 of baseline. The results were consistent with similar observational studies. The results indicate that Cannabis effects are significantly greater in some scales than might be seen in traditional clinical trials. Double-blind, randomized trials are best used to evaluate specific formulations for specific indications. The observational studies use a broader view and establish that patients use Medical Cannabis in dose-dependent fashion because the benefits of use exceed the harms. Nancy Reagan died on March 6, 2016, a couple of years before this most recent Medical Cannabis study launched. Would she have said yes to Medical Cannabis after reading these results? In hindsight, the fundamental lesson should be that actresses, politicians, and government regulators are not always the best resource for improving Quality of Life. The community discovered Medical Cannabis despite contradictory rhetoric and traditional evidence. Community derived information is a pertinent resource. When it comes to Medical Cannabis the best advice might be to “Just Say Yes”. |
AuthorJean Talleyrand, M.D., Archives
September 2023
Categories |
Mailing Address: MediCann 1336 Willard Street, C • San Francisco, CA 94117
Important Disclaimer!
The information contained in this site does not intend to replace any medical advice or care by a trained physician.
Any use of this information is solely the the responsibility of the user.
Important Disclaimer!
The information contained in this site does not intend to replace any medical advice or care by a trained physician.
Any use of this information is solely the the responsibility of the user.
© COPYRIGHT 2015. ALL RIGHTS RESERVED.











 RSS Feed
RSS Feed