|
A syndrome is a collection of symptoms that frequently occur together. Tourette’s Syndrome is characterized by sudden, repetitive, rapid, unwanted movements or vocal sounds called tics. Many people associate Tourette’s with outbursts of obscene or socially inappropriate words. Although only one third of people with Tourette’s make obscene remarks. Those who have outbursts find it difficult to deal with public places, school, work, or even home. Just getting through the day can be excruciatingly difficult. Doctors previously thought that Tourette’s was a psychological disorder. Today, most scientists agree that Tourette’s is a neurological disorder with unknown causes.
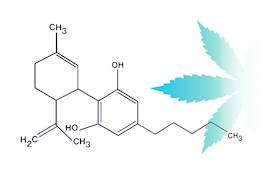
Tics come and go over time. They first appear between the ages of 5 and 10, usually in the head and neck area. Motor tics typically appear before vocal tics or outbursts. The tics usually get worse in the early teen years and become more controlled by the late teens or early 20s. Tics worsen with excitement or anxiety and improve during calm or focused activities. Imagine trying to calm your excitement or anxiety as a teenager. Canadian researchers performed a double-blind, randomized, placebo controlled, cross-over study of nine people with Tourette’s. In prior studies, patients had reported a reduction in tic severity, improved sleep, and improved mood after using Cannabis. This study controlled the type of Cannabis and dosage used. Each participant vaporized ¼ gram of either Type I, II, III, or placebo Cannabis flowers once every two weeks. The Type I Cannabis had only 10% THC, Type II had 9% each of THC and CBD, and Type III had 13% CBD with very little THC. Four different survey scales were used to assess the frequency and severity of the tics after Cannabis use. The Type I (or 10% THC) flowers worked best. Type II (or 1:1 ratio THC and CBD) were a little less effective than Type I. Type III CBD flowers did not have any significant effects. Type I and II Cannabis improved urge for tics, symptoms of distress, and overall well-being. Type I flowers also had more cognitive and psychological adverse events. The researchers admitted that it was difficult to draw conclusions from a small sample of participants. MediCann has evaluated a handful of patients with Tourette’s. Their ages range from 18 to 46. On average, they smoke ½ gram of Tyle I Cannabis (closer to 20% THC) 3-4 times per day. Some just smoke 1 time per day and others may smoke up to 8-10 times per day. One patient, the 18-year-old, tried a CBD tincture without success and is next planning to try a 1:1 THC-CBD tincture. Outside of the 18-year-old, they all report improved symptoms with Cannabis use. When it comes to Cannabis, collecting real-world data complements traditional study design. Non-interventional studies of Tourette’s demonstrate significant improvement with Medical Cannabis. The studies illustrate a wide range of dosage and variable experiences with Cannabis. They highlight that Cannabis is not a one-size fits all medicine. “Medical Students Have Little Knowledge About Cannabis, Study Finds,” an article published in Cannabis Health by Joe Roberts describes a study about medical student Cannabis education in the US
Researchers from Nova Southeastern University and Florida Atlantic University published the results of a qualitative study on the perceptions of Cannabis by medical students in Florida. The goal of the study was to identify themes shared by the students that may be helpful in designing future curricular on Medical Cannabis. This study was one of the first to use qualitative interviews to explore student perspectives on Medical Cannabis Qualitative studies focus on the “why” rather than the “what”. They use semi-structured questions in a natural setting to create an in-depth conversation and understanding of the topic. In this study, a total of 83 medical students in eight focus groups were questioned through ZOOM. The questions were designed to get an understanding of 1) beliefs about the therapeutic benefit of Cannabis 2) general knowledge about Cannabis and 3) the potential role of the physician. Each focus group lasted between 60 and 75 minutes. Most of the medical students were in favor of re-scheduling Cannabis to something less than Schedule I. Most were able to name a symptom or condition that might benefit from Cannabis. And only a few could name a health condition that was contraindicated or had no benefit with Cannabis use. Students did have concerns about the potential for Cannabis addiction and long-term effects. Most said their source of information came from friends and family or through social media. The two medical schools did not have courses on Cannabis or the Endocannabinoid System. The students were able to identify conditions, including cancer, AIDS, pain management, irritable bowel, multiple sclerosis, and others., that might benefit from Cannabis. They also expressed concerns about the potential harms of Cannabis. “A lot of people recommend chilling out with Medical Cannabis,” said one student, “but it actually can evolve into a panic attack.” Student perspectives ranged from concerns about addiction to a lack of trust in patients knowing what was medically best with their Cannabis use. The researchers concluded that most students had erroneous beliefs about Medical Cannabis. They used unreliable sources of information and had mixed attitudes about legalization. The students also tended to confuse Medical Cannabis use with recreational use. The researchers described the way the students spoke about Medical Cannabis as “unsettling” and based on “unsubstantiated authority.” Despite their confusion, the students were all interested in learning more. Most felt that their medical school should offer Medical Cannabis training. They noted that even if a state does not have medical Cannabis laws, they are likely to run into patients using Cannabis sometime in their career and would like to be prepared. It’s been over 40 years since the Endocannabinoid system was discovered. Typically, new discoveries don’t take long to be included in a medical school curriculum. Outside of the stigma of Cannabis, there are concerns that science has not yet tackled the hurdles presented by variable, multi-agent, Cannabis medicines. There are those who make the argument that Medical Cannabis may require changes in the way we approve medicines. Years of patenting single or dual agent cannabinoids have not captured the revenue and presumed effectiveness of increasingly popular Cannabis. There is also some indication that pharmaceutical industry is losing billions in stock value to burgeoning Cannabis sales. At the same time, pharmaceutical industry’s influence on medical education, may be slowing progress toward implementing changes to medical Cannabis curricular. It’s a perfect storm that must eventually be resolved. |
AuthorJean Talleyrand, M.D., Archives
September 2023
Categories |
Mailing Address: MediCann 1336 Willard Street, C • San Francisco, CA 94117
Important Disclaimer!
The information contained in this site does not intend to replace any medical advice or care by a trained physician.
Any use of this information is solely the the responsibility of the user.
Important Disclaimer!
The information contained in this site does not intend to replace any medical advice or care by a trained physician.
Any use of this information is solely the the responsibility of the user.
© COPYRIGHT 2015. ALL RIGHTS RESERVED.



 RSS Feed
RSS Feed