|
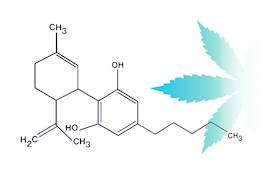
By Jean Talleyrand, M.D. and John S. Abrams, Ph. D. In times of crisis it is customary to “sound the alarm”. However, an alarm with solution is significantly more effective and worthwhile than an alarm alone. The worldwide effect of COVID-19 is alarming. In the U.S., over 20% of the tested population has contracted the virus. As COVID-19 and likewise SARS produce acute respiratory symptoms, it is often mistakenly assumed that people with chronic obstructive pulmonary disease (COPD) are at higher risk for contracting the infection. Data on the prevalence of COVID-19 and SARS infection shows a lower percentage of infection in people with COPD compared to the general population.1 However, common sense prevails. Despite the lower prevalence of disease there is a five-fold increase in severe outcome in those patients with COPD who have contracted the virus.2 Smoking Cannabis alone has not been associated with an increased risk of developing COPD.3 However, smoking both tobacco and Cannabis is associated with an increased risk or respiratory symptoms and COPD.4 Dr. Jeffrey Block, Executive Board Member of the American Society of Cannabis Medicine suggests that in this time of crisis safer alternative methods of using Cannabis are likely to “save lives”. Historically, Cannabis tincture and Cannabis water decoction formulations have been reported effective ways of using Cannabis.5,6 As well; modern state regulatory standards allow Cannabis to be available in capsules and gummies with incremental doses of 2.5mg, 5 mg, and 10 mg of THC. Additionally, there is growing recognition of the efficacy of the other major cannabinoids in Cannabis, THCA, CBD, and CBDA, all of which demonstrate therapeutic potential without psychoactivity. Medical Cannabis use is a recently developing clinical practice. Due to the Controlled Substances Act, years of Cannabis prohibition have impeded medical understanding of the therapeutic benefits of Cannabis active ingredients. A March 2020 review of clinicaltrials.gov identifies 106 completed Cannabis clinical studies. Seventy studies (66%) involve Cannabis 1 Halpin, DG et al. Do Chronic Respiratory Diseases or their Treatment Affect the Risk of SARS-COV-2 Infection? The Lancet Respiratory Medicine Comment 2020 Apr 03 2 Lippi G et al. Chronic Obstructive Pulmonary Disease is Associated with Severe Coronavirus Disease 2019 (COVID-19). Respiratory Medicine 2020 Mar 24 3 Tashkin, D. Does Smoking Marijuana Increase the Risk of Chronic Obstructive Pulmonary Disease? Canadian Medical Association Journal 2009 Apr 14; 180(8); 797-798 4 Tan WC et al. Marijuana and Chronic Obstructive Pulmonary Lung Disease: A Population Based Study. Canadian Medical Association Journal 2009; 180(8); 814-820 5 Bridgeman, M et al. Medical Cannabis: History, Pharmacology and Implications for the Acute Care Setting, Pharmacy & Therapeutics 2017 Mar; 42(3); 180-188 6 Boekhout van Solinge, Tim (1996), Ganja in Jamaica. Amsterdams Drug Tijdschrift, nr 2, December 1996, pp. 11-14. Abuse, Cannabis Use Disorder, Cannabis Withdrawal and Substance Use Disorder.7 The National Institute on Drug Abuse (NIDA) advances science on the causes and consequences of drug abuse and addiction. NIDA has actively funded the majority of Cannabis research during prohibition, which has left an imbalance of information on the cumulative effects of Cannabis. Dr. Nora Volkow, director of NIDA, identifies persons with addictions and drug abuse as vulnerable to poor outcomes from COVID-19. Indeed, persons with addiction are well known to have comorbid behaviors, which makes them vulnerable to illness.8 However, the tide has turned in regards to Cannabis use. Cannabis can no longer be considered just an illicit drug. It is increasingly appreciated that the Endocannabinoid system (ECS) plays a key role in shaping the direction of the immune response. Cannabinoids (such as THC and CBD present in Cannabis products) may be differentially influencing the overall type of immune effector function 9,10. This can result from a push more towards a cell-mediated virus-killing effector function, or towards a protective or neutralizing antibody response. In this era of the COVID- 19 pandemic, it is key that we understand the Cannabinoid tools that we currently have at our disposal. The “medicalization” of Cannabis allows access to products with identified active ingredients and recommends guidance to their use by physicians. In this time of crisis when infection, stress, anxiety, and insomnia are at increasing prevalence, the responsible use of Cannabis presents a solution for consideration. Jean Talleyrand, M.D. is Chief Medical Officer of MediCann, a medical Cannabis education organization and the Clinical Endocannabinoid System Consortium, a research organization John S. Abrams, Ph.D. is Chief Science Officer of the Clinical Endocannabinoid System Consortium, a research organization 7 Talleyrand, J. Review of Completed Cannabis Studies with Results (clinicaltrials.gov). The Clinical Endocannabinoid System Consortium www.thecesc.org; 2020 Mar. 8 Miller, NS et al. Comorbid Cigarette and Alcohol Addiction. Journal of Addictive Disease. 1998; 17(1); 55-66 9 Yuan M1, Kiertscher SM, Cheng Q, Zoumalan R, Tashkin DP, Roth MD. Delta 9- Tetrahydrocannabinol regulates Th1/Th2 cytokine balance in activated human T cells. Neuroimmunol. 2002 Dec;133(1-2):124-31. 10 Nichols, James M. and Kaplan, Barbara L.F. Immune Responses Regulated by Cannabidiol. Cannabis and Cannabinoid Research Vol. 5, No. 1 ReviewsOpen AccessOpen Access license |
AuthorJean Talleyrand, M.D., Archives
September 2023
Categories |
Mailing Address: MediCann 1336 Willard Street, C • San Francisco, CA 94117
Important Disclaimer!
The information contained in this site does not intend to replace any medical advice or care by a trained physician.
Any use of this information is solely the the responsibility of the user.
Important Disclaimer!
The information contained in this site does not intend to replace any medical advice or care by a trained physician.
Any use of this information is solely the the responsibility of the user.
© COPYRIGHT 2015. ALL RIGHTS RESERVED.

 RSS Feed
RSS Feed