Patients Grow to their NeedsThat’s right. Medical Cannabis patients in California can grow to their needs, NO LIMITS.
California voters did something right when they enacted Prop 215. The 1996 voter initiative provides a defense for medical patients and their defined caregivers who grow and possess Cannabis at any amount for medical purposes. Titled the “Compassionate Use Act of 1996”, Prop 215 identifies medical conditions as the underlying defense for growth and possession of Cannabis. The qualifying medical conditions need to be confirmed by physician evaluation. As well, the physician is responsible for guidance. Prop 215 authors, Dennis Peron, Valerie Corral, Dale Gieringer, Tod Mikuriya, and many more, formed an all-star cast of compassionate professionals who chose not to describe Cannabis as a commodity in the law. They emphasized COMPASSION for patients. There are many who recognize the poor job California regulators have since done in regulating Cannabis. A lot of the problems are attributed to Prop 64, the “Control, Regulate, and Tax Adult Use of Marijuana Act”. Like a tenant of the Evil Empire, the Prop 64 initiative describes Cannabis as a commodity and benefits large corporate growers. As a result, many small crop Cannabis farmers have shut down their licensed operations and sold their farms. Currently, the best access to quality, low-cost medical Cannabis remains the 215 recommendation which allows patients to grow their own. Confusion Continues “How many plants can a qualified medical cannabis user grow in California? Ask law enforcement or various state and county departments, and each agency, in some cases, each individual within each agency has a different answer,” writes Nichole Norris in the Redheaded Blackbelt. Apparently, county officials are confused. Humboldt County Sheriff deputies and code enforcement officers have been caught on camera saying, “There is no medical anymore,” and “215 doesn’t matter.” However, in an interview with Ms. Norris this summer, Humboldt County Sheriff Billy Honsal recognized medical cannabis laws. Sheriff Honsal believes Prop. 215 was not written well. However, he understands that if someone is growing more than six plants deputies must look at the 215 documents. Adding to the confusion, Humboldt County Building and Planning Department operates on different limits allowing 100 sq-ft, 200 sq-ft, or 400 sq-ft depending on lot size. Cannabis expert and local criminal defense attorney, Eugene Denson, writes “It is important for the Sheriff, the Code Enforcement Unit, and other county officials to understand what is allowed under existing law because I believe they are presently violating the law… due to a mistaken opinion of what the laws of California allow. These actions make the county liable for damages and other legal remedies available to patients.” Past medical patients uprooted their lives and moved to Humboldt County to benefit from a favorable Cannabis environment. Some patients see Cannabis as the plant that saved their lives from the suffering of chronic illness.. Humboldt County is well known as an epicenter of Cannabis. The tenacity and persistence of Emerald Triangle inhabitants to grow their own Cannabis despite the laws enacted to "control, tax, and regulate" has started a movement to world wide legalization.. However much regulators put their hands out panning for cash to fill government coffers, they cannot bully the medical Cannabis patient. Thankfully, the authors of Prop 215 saw Cannabis as more than a commodity. As a result of their incredible foresight, medical Cannabis patients can continue to produce their own medicine and the legacy the personal medical Cannabis garden continues. Sometimes there is no solution to a problem. Chronic pain is like that. You don't get rid of it. You just learn to live with it, doing the small things to make the day go by with some small reward of laughter. - Dr. T  Why continue living? Not that there is much choice in the matter.
Thoughts on PAIN! I have a rather too intense, intimate and enduring personal relationship with pain that continues to intensify. Pain is a unique experience as unique as the individual experiencing the pain. Pain is more than physical. It is emotional and psychological as well. Never belittle another person’s pain. Never consider your pain to be greater than anyone else’s. Invisible does not mean nonexistent. Pain only kills if it causes shock and death is due to shock left untreated. Pain that intensifies over time can seem to endure for eternity. The desire for the end of existence can result from acute chronic pain lasting decades and other major complications of life. As if there is life without complications. Death does not guarantee the end of pain and suffering. Pain is part of the shit that happens to the living due to living. It is thought that the dead do not experience pain. Pain is the hard way to learn important life lessons. Pain is not something to be distributed, propagated, shared or spread. Empathy is acceptable; sympathy is not. I do believe that I have warned you upon several occasions that I have a twisted sense of humor. -Anonymous A After being with hundreds of dying folks, my belief is that this human experience is the bottom rung of the ladder and that as spiritual beings it only gets better! We are spiritual beings having a human experience, not the other way around.
-Anonymous B  I'd like to introduce you to “Flore”, a newly opened Cannabis retail store. Flore is located at the historic corner of Noe and Market in San Francisco’s Castro neighborhood. More than 25 years ago, Brownie Mary handed out Cannabis infused “treats” to AIDS patients on this corner. Just down the street, Dennis Peron’s Cannabis Buyers Club became the world’s first medical Cannabis dispensary. About the same time, I consulted my first medical Cannabis patient just a few blocks away. Northern California has been involved in a Cannabis culture since before the "Summer of Love". In the 1960s, anti-war and civil rights were at the forefront of social discussion and debate. Considering current events, it amazes me how history repeats itself. Cannabis stood for rebelliousness, iconoclasm, and radicalism. Although we may have changed, the plant hasn’t changed. As a community, perhaps we have evolved to understand Cannabis heals the prevalent disorders of the day. After Cannabis and other psychedelic experiences, Harvard psychologists Timothy Leary and Richard Alpert questioned the status quo. Their experiences with Cannabis as a mild mind-altering escape from reality gained popularity. Dr. Leary and Dr. Albert reinforced the prevailing notion that science instructs wellness and medicine. Today, communities find that “turning on” to Cannabis also manages pains, helps addiction, improves sleep, and relaxes a person from the mental and physical stressors. Cannabis bridges the herbal apothecary of the past to the pharmacy of the future. Our work at the CESC, a nonprofit Cannabis research organization, has always sourced community wisdom. Federal and state regulatory efforts address limited challenges presented by Cannabis. Relying on top down federal and state guidance does a disservice to a community that has used Cannabis for decades. Yet, our community is thirsty for knowledge. Although we have experienced relief of aches, pains, and stressors, we want to understand which Cannabis products give energy, and which helps with a good night’s sleep, which stimulates hunger, or, yes, even arousal. Dr. Abrams and I started our clinical research by examining how communities use aroma to make distinction between Cannabis flowers. The investigation eventually led to chemical characterizations of Cannabis flowers and predicting the "Sativa" vs "Indica" effects. Our studies are a paradigm shift to traditional FDA clinical studies. Using community sourced data, we learn quickly and at very little expense. Flore sits at ground zero of the Cannabis culture in northern California. It will be the place where CESC launches its next phase of studies on Cannabis dosage and efficacy. “Our initial work focused on Cannabis flowers. Today we are ready for a new phase of study,” explains Dr. Abrams. “We want to dive into a broader side of Cannabis - processed (non-flower) products.” Processed Cannabis products allow choice, provide variability, and are amenable to scientific precision. As well, consumers are interested in reliable and consistent Cannabis products that result in characteristic anticipated effects. As we mature, the Cannabis industry matures, where getting “high” is just one of many available choices at a Cannabis dispensary. The CESC believes that effect claims are possible through observational study. In fact, large cohort Cannabis observational studies may be more predictive than smaller double blind randomly controlled trials. With help from the community, the CESC will make effect claims available to the public for any product available at Flore. Our mission is to provide information for each Cannabis product categories (gummies, vape carts, topical salves, etc.). We see this information as critical for both consumers and the industry. Dr. John S. Abrams and Dr. Jean Talleyrand are co-founders of the CESC Flore is located at 258 Noe St, San Francisco, California Considering that the Russian-Ukrainian war, misaligned SCOTUS decisions, and an insurrection are the dominant topics in the news, I will highlight this holiday with a promise to evolve with more compassionate and responsible access to Cannabis
I’ll start by paraphrasing a story by Will Fritz of the NY Cannabis Insider titled, “Another medical marijuana patient describes ongoing problems with price, service, and access”. The story is part of an ongoing series that elevates the voices of NY’s Medical Cannabis patients. Shortly after New York legalized recreational Cannabis, patients and advocates began sounding the alarm about the state’s handling of medical Cannabis, alleging NY’s medical program was being left to rot while regulators focused instead on the adult-use market. Christopher, a 25-year-old medical Cannabis patient from Long Island uses Cannabis to treat PTSD. Christopher says he has trouble getting accurate and helpful information from “budtenders” at medical Cannabis dispensaries. When asking for recommendations on what products he can use to best treat his condition, he says he’s often met with little more than a shrug. “It’s like going to CVS, but the people at the pharmacy are like the people at the checkout. In New York it’s like, they’re just here to sell the stuff,” says Christopher. “You’re working with medical patients who rely on this medication — there should be a level of professionalism.” He has also encountered privacy issues at his main dispensary, where his PTSD is plainly labeled on the outside of the package when he purchases products. “They’ll put your issue on your package, right on display for everyone,” says Christopher. Christopher also complains that it’s difficult to find affordable dispensaries. He has visited other states where the pricing is significantly cheaper. “When I went to Maine, I was able to get a full gram cartridge for like, $15.” “The same product,” he says, “would be as much as $100 more at his usual dispensary in New York. Christopher acknowledges that it makes some sense that a state with a higher cost of living in general is going to have more expensive medical Cannabis than in states where it is less expensive to live. Still, the difference seems outrages. “Is it $100 difference?” says Christopher. “I don’t think so.” Like other patients, Christopher also complains about delays and problems with the Office of Cannabis Management, especially regarding the fact that home cultivation has not been adopted. “It’s crazy that you still can’t grow your own,” says Christopher. “What’s the OCM going to do, they’re going to break into my garage and take it?” High prices, less accessible products, and a lack of professionalism are all issues that are ongoing in the Cannabis industry. The re-introducing of Cannabis as a viable and valuable commodity started with compassion and an action to help others. A Cannabis users community and industry started the movement to legalization. Law makers did not initiate regulatory changes, the people did. With supplies at a surplus, it’s up to the people to drop prices through industry practices. Education is accessible and professionalism is an attitude that are not costly. For the sake of the suffering who inspired us to re-introduce Cannabis to the world, it’s up to the people through community and industry to evolve to a better place It’s been more than 25 years since Californian’s passed Prop 215. Today, even states like Texas and Georgia have enacted compassionate use laws. That’s right compassion. That’s how it all started. People who were dying with overwhelming sickness needed help. Modern pharmaceutical drugs were not successful, their side effects causing more problems than they solved. We have evidence of an opiate crisis. We have intractable nausea and vomiting from Cancer chemotherapy. There are people anxious or depressed after traumatic life experiences or unable to sleep and addicted to sleeping pills. All these problems are addressed by allowing people to grow Cannabis, a plant that humans have cultivated for thousands of years.
Today I learned that the Humboldt County Director of Planning and Building ordered a deputy sheriff to tear down the personal garden of one of my patients. He is sick and needs medicine. An annual report from DEA’s Domestic Cannabis Eradication/Suppression Program says that the agency confiscated more than 5.5 million Cannabis plants and arrested approximately 6,600 people over Cannabis in 2021. That’s a 22% increase in the number of confiscated plants and a 32% increase in the number of people arrested. It’s both funny and sad when you think about. Humanity prides itself on having large brains and being the thinking animal. If we are so thoughtful, why do we prohibit or control the cultivation of a plant that we find useful? Somewhere in the forest, animals with much smaller brains are shaking their heads and laughing at the same time. You might think of having a personal garden. The idea of enjoying sweet fruit and crisp vegetables from your own garden does not cause fear or panic. But, if you think of incorporating Cannabis into your garden, you must pull out the rule book and worry about your neighbors. How many plants are OK? What, I can’t just grow what I want or need? “At a time when the overwhelming majority of voters support legalization, and when more and more states—and even members of Congress—are moving toward this direction, it is troubling to see federal agents and their local partners reversing course and reinvigorating their marijuana (Cannabis)-related enforcement activities,” says Paul Armentano, deputy director of NORML Northern California is notorious for its stance against Cannabis prohibition. People are either from there or have moved there to cultivate Cannabis. They escaped up winding mountainous roads and disappeared among the redwoods to grow the weed. Elected officials looked the other way or sometimes even participated in Cannabis cultivation. With the repeal of prohibition, one might expect the inhabitants of northern California to be dancing in the streets. But ignorance and greed persist and the war on Cannabis continues. Cannabis is a plant that grows easily for the benefit of humans. We are thankful to have powerful medicines, strong fibers, and nutritious oils from such a wonderful plant. Those elected officials and henchman-like law officers that continue to insist on controlling the cultivation and restricting sharing of this earthly bounty for power and gain must go. The war on Cannabis continues and the personal Cannabis gardener is the foot soldier. In health or in defiance, put a Cannabis plant in your garden today and signify that any attempt to obstruct and dominate over the planting of a seed will never succeed. A recent study by investigators at the University of New Mexico, Department of Psychology, reveals that Cannabis users prioritize Empathy, Moral Fairness, and Moral Harmlessness. The study, titled “Cannabis Consumption and Prosociality”, was published in Nature Scientific Reports. “Prosociality” refers to the intentional act of advancing the well-being of others.
Previous studies have suggested an association between Cannabis use and antisocial behavior. For example, a study of people with a criminal history of aggression proposes that their Cannabis use is a predictor of their aggressive behavior. Another study of men arrested for domestic violence links Cannabis use to future violence. These studies describe the behavior of lawless and disruptive Cannabis users. However, they don’t lend insight to Cannabis use among healthy populations. In response, psychologists decided to evaluate healthy Cannabis users. They measured the traits of 146 young adults between the ages of 18 and 25 using validated social psychology scales. Participants’ urine was tested for THC and they were asked if they had recently used Cannabis. Approximately half of the participants had recently used Cannabis. Those with THC in their urine had higher “prosocial” scores compared the THC-free cohort. THC positive females scored higher on measures of aggression and THC positive males scored higher on measures of agreeableness. It's important to note that the study found no difference in measurements of anger, trust of others, emotional stability, openness, principles of respecting authority, and preserving the concept of purity. The authors explain that Cannabis is often consumed to reduce feelings of anger and aggression. Animal and human studies have shown that, unlike alcohol, Cannabis intoxication results in a decrease in aggressive behaviors. Observational studies indicate that Cannabis users are less irritable, agitated, and stressed. With increasing access to Cannabis, it’s important to understand what happens to Cannabis use in healthy populations. This study consisted of undergraduate students at University of New Mexico. These students were without chronic health conditions. They also likely have similar social environments. A study of this population explains an association of Cannabis use for a specific group of people. Nevertheless, the results add to growing evidence that Cannabis use can add benefit to healthy populations. Similar studies can be applied to other healthy populations.  This story is by Sean Teehan from NY Cannabis Insider On the morning of the 2005 Rochester Marathon, Brian Lane considered not showing up for the race. Juggling his job with the U.S. Postal Service, raising two children, and going through a divorce took the wind out of his sails, and running a long-distance race felt like a chore. But people were expecting him to be there, so he dragged himself out of bed, took four heavy bong rips and made his way to the starting line. Lane ran the 26-mile race with a time of 3:11:23, finishing 16 out of 658 runners and qualifying for his first Boston Marathon. Lane is owner and compliance officer at Rochester based hemp processing company NOWAVE and host of Hempthlethics, a podcast about incorporating Cannabis into exercise. “I think it’s the most under talked about niche,” Lane told NY Cannabis Insider. A subset of users some call “cannathletes” are becoming increasingly visible. In a University of Colorado survey of 600 Cannabis users, 80% reported using Cannabis before, during, and after workouts. “Everyone who is a regular Cannabis user that I have brought onto my show, they’re all active,” says Lane. “There’s nobody sitting on their couches doing nothing.” Lane’s long-term goal is to release a line of products that cater to the cannathletic market. Cannabis companies currently serving the athletic market include Offfield, which makes gummies, soft drinks, and other products that include THC. Another is WannaFit, who makes products that are infused with THCv Josiah Hesse, author of the book Runner’s High, dives deep into how both elite athletes and weekend warriors use Cannabis. “The market for it is endless,” says Hesse. “There’s no demographic that Cannabis doesn’t reach, young people, old people, all races, all political affiliations, all economic backgrounds.” Dr. Ethan Russo agrees. “Some uses of Cannabis in conjunction with exercise already have pretty strong scientific backing. THC and CBD have pain killing and anti-inflammatory effects that can help following a workout. However, the idea that Cannabis can help people during a workout is more nuanced.” He recounts his own experience of skiing under the influence of Cannabis. “Being able to key into the rhythm is a benefit,” says Russo. I really like this idea of combining Cannabis and athletics. I usually consult patients who are using Cannabis for chronic pain or other illness. It’s refreshing to know Cannabis is also used for wellness activities like workouts. Cannabis is not always about the party and we don’t have to wait and get sick before using Cannabis. Using Cannabis for wellness is proactive. I also think the Cannabis industry should promote their own Cannabis athletic events. We could raise awareness for elite athletes like Sha’Carri Richardson, the sprinter who was banned from the Tokyo Olympics. Athletic events are a good way to highlight the positive aspects of Cannabis use. Cannabis consumers would be able to buy directly from cultivators at farmers markets, just like they do for produce, under approved legislation, AB 2691, by the California state Assembly. The state Committee on Business and Profession recently approved the bill, which now has to clear the Assembly Appropriations Committee and the full Assembly Chamber and then go through the Senate before reaching the governor’s desk.
Cultivators have had financial challenges since passage of Prop 64, the Control, Regulate and Tax Adult Use of Marijuana Act. Wholesale prices farmers receive for outdoor grown Cannabis averaged $488 per pound according to research from Cannabis Benchmarks. This is a 55% drop from 15 months earlier. Kristen Callahan, owner of Magic Meadows Farms in Middletown in Lake County is quoted by the Sacramento Bee, “This is an important first step that will help our cash flow by being able to sell directly at farmer’s markets.” Several dozen farmers that showed up for the committee vote were pleased. They see the direct sales as a beginning of Cannabis tourism in California. Visitors could sample different varieties of Cannabis, similar to what they do at a winery The bill’s opponents are dispensary owners, who are concerned about competition. Another of the bill’s opponents, Assemblyman Phillip Chen, states, “As I represent Orange County, there will be an over saturation of these retailers in my communities.” The bill sponsor, Assemblyman Jim Wood, D-Santa Rosa, countered that the legislation was about, “giving the little guy a chance.” The farmers insist that allowing consumers to sample their product at farmers markets will only promote Cannabis, benefiting all the Cannabis consuming community. Farmers can show their products currently at farmer’s markets, but the system doesn’t allow them to make a direct sale. Consumers must go to another booth at the market and buy Cannabis products from a licensed retail operator. "I think it's super, super awesome and I like that they're kind of getting rid of that guilt or that dark cloud that they have around the whole weed industry,” Davis resident Crystal Molina said. Since recreational cannabis was legalized in California the morning of January 1, 2018, there have been only three outdoor events in San Francisco with legal cannabis sales. And all three were in Golden Gate Park — Outside Lands 2019, Outside Lands 2021, and the 2022 4/20 Hippie Hill celebration from two weeks ago According to SFiST, Permit applications have been submitted to bring legal cannabis sales to Carnaval SF on May 28-29, and there’s a high likelihood that Carnaval will be the first California street fair with legal, regulated cannabis use. 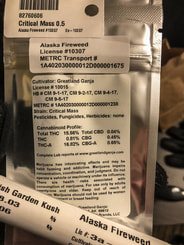 As if California Medical Cannabis patients didn’t suffer enough. Apparently, other states have not learned from California’s mistakes. The headline from Ganjapreneur by TG Branfalt is “Medical Cannabis Strained by Adult-Use Sales in New Mexico” New Mexico medical Cannabis patients are expressing frustration. Increased demand from adult-use sales is straining the New Mexico Cannabis supply. On April 1st, licensed Cannabis dispensaries in New Mexico started adult use sales one year after legislators passed an adult use legalization bill. The roll-out was expected to be gradual since many producers and retailers were building out their operations or just getting municipal approval. The expectation didn’t account for consumers. The state Cannabis Control Division says New Mexico sold over $8 million in adult use Cannabis in just two weeks after legalization. KOB 4 Eyewitness news reports that, despite the large sales, medical Cannabis demand remains high. Stephanie K, a long-time medical Cannabis patient says, “They’re telling us we should keep our cards (Referring to medical Cannabis identity cards) even though it’s recreational. For what reason? What perks are we getting? We don’t get to get in line in front of anybody, we don’t get to pay less, we don’t get better weed. No, we get nothing.” Some New Mexico Cannabis retailers have tried to look out for patients. Ellie Besancon, Executive Director of Green Goods, wants to create separate display cases for recreational products and medical products. But she feels patients still have a frustration level. They already know what they want and the lines are long. MJBiz Daily reports that Texans may be playing a role in consuming New Mexico Cannabis. “Our studies show that 40% to 42% of all adult-use cannabis will be derived from out-of-state purchases, particularly Texas,” says Duke Rodriguez, CEO of the state’s largest cannabis company California went through its own growing pains after enacting adult-use Cannabis laws. In California, consumer prices remain high despite a supply glut. A significantly large percentage of Cannabis sales are believed to remain in traditional markets. On the East Coast, New York, New Jersey, and Connecticut will be selling adult use Cannabis soon. As of April 21st, New Jersey has already started. Can they learn from the issues western states are experiencing or will medical Cannabis patients suffer similar access issues? Medical patients typically have a different need and urgency for Cannabis. "I don't do it to party. I don't do it to go out and dance. I don't get high. I don't laugh. I do it because it makes my pain go away,” said Stefanie. now that adult-use has arrived, the shops are only concerned about “money, the dollars.” Once again, it seems to me that legislators have forgotten about COMPASSION for patients for the money. What do you think? This story was published in Ganjapreneur on March 8, 2022, by TG Branfalt. Their headline is “Few Parents know about CBD use in Children” A recent poll by the University of Michigan’s Mott Children’s Hospital sampled 1,992 parents with at least one child between the age 3-18. Most parents polled (80%) either did not know much about CBD use in children or never heard of it prior to the poll. I might have stopped the poll right there. Apparently, it is of some value to the authors to ask parents about something they don’t know much about. Seventeen percent of parents reported knowing something about CBD and children. Only three percent said they knew a lot. Despite not knowing about CBD, 73% of parents optimistically thought CBD might be a good option for children when other medications don’t work. The factors that are important to parents in deciding whether to give CBD to children are its side effects. 83% thought CBD products should be regulated by the FDA, and about three quarters say CBD for children should require a doctor’s prescription. About one third thought taking CBD is basically the same as using marijuana. (By marijuana, I assume they mean Cannabis with more than 0.3% THC.) Most (93%) parents have never given or considered giving their child a CBD product. 2% have given their child a CBD product, while 4% have considered giving CBD to their child; 1% say their child has used CBD without their permission. Among the small percentage of parents who have given or considered giving CBD to their children, the most common reasons included anxiety (51%), sleep problems (40%), ADHD (33%), muscle pain (20%), autism (19%), and to make their child feel better in general (13%). This poll highlights the limited knowledge that most parents have about CBD and children. Parents might do anything for a sick child, especially when other medications are not working. Would you give a sick child CBD? Would you give THC? |
AuthorJean Talleyrand, M.D., Archives
September 2023
Categories |
Mailing Address: MediCann 1336 Willard Street, C • San Francisco, CA 94117
Important Disclaimer!
The information contained in this site does not intend to replace any medical advice or care by a trained physician.
Any use of this information is solely the the responsibility of the user.
Important Disclaimer!
The information contained in this site does not intend to replace any medical advice or care by a trained physician.
Any use of this information is solely the the responsibility of the user.
© COPYRIGHT 2015. ALL RIGHTS RESERVED.




 RSS Feed
RSS Feed